Reading time: 5 minutes
Patty Spears
For many years there has been a lot of talk about the promise of using a mere blood sample to detect cancer in your body. There are many different approaches and tests that have been developed. One type of test coming to the forefront looks for circulating tumor DNA (ctDNA). Every cancer cell has unique DNA. When the cancer cells die, this DNA is released into the blood. This is called circulating tumor DNA (ctDNA). Focusing on ctDNA, let’s look at the promises and the challenges of using this new test to detect cancer.
What will it take to get it over the finish line? Well, it’s complicated. There are some basic concepts to know in order to understand the best way to use ctDNA testing in blood samples during cancer care.
Type of cancer: It has become clear that not all cancers are the same. Lung cancer is not breast cancer; breast cancer is not colon cancer. The amount, type and meaning of ctDNA in different cancers may not be the same.
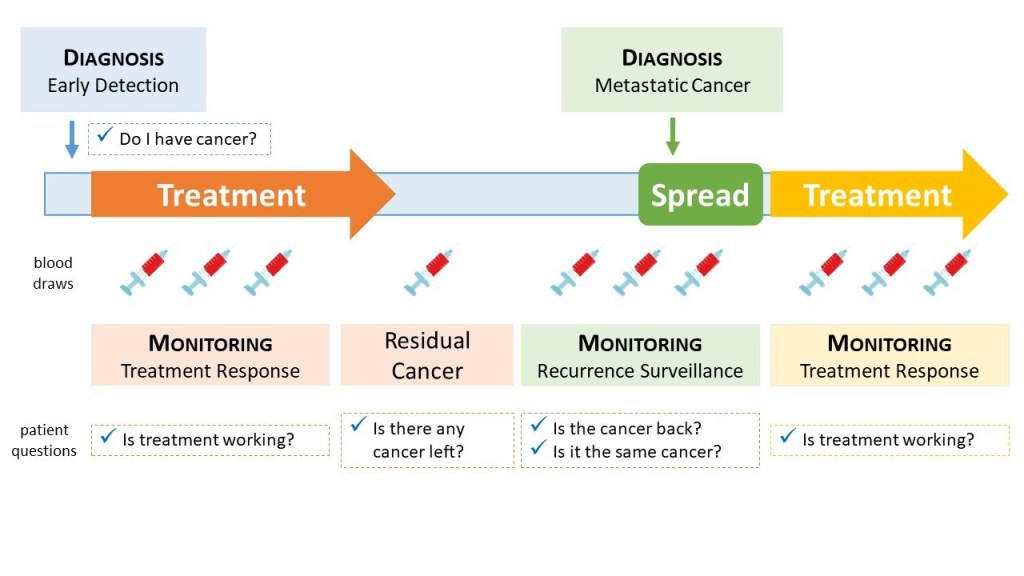
When the test is done: ctDNA is being looked at during every step in cancer care, even before cancer has been diagnosed (see Box A).
Before Diagnosis: Looking for ctDNA before someone knows they have cancer will be challenging. It is like looking for a needle in a haystack. There will be fewer positive tests in the general population. This is a high bar to get over. If there is ctDNA present, now what? This is where biology and technology have to be in sync.
NOTE: There will be a lot more negative tests than positive tests and the positive tests must be correct. An incorrect positive test will result in unnecessary follow-up testing. The idea of possibly having cancer will increase anxiety of the person until the follow-up testing proves there is no cancer present.
Early Cancer and Treatment: Looking for ctDNA when diagnosed will determine if ctDNA is present or not before treatment begins. Then seeing what happens to it during and after treatment has the potential to change cancer care. “Is it all gone? Has it increased or decreased? Do I need more treatment?”
NOTE: This is where there are differences depending on cancer type, risk and stage. The chances of ctDNA being seen in a blood sample is more likely in those who have a higher risk of recurrence.
After Treatment: Looking for ctDNA after treatment can be done to monitor for a recurrence. “Has my cancer come back and spread to other parts of my body?” This is the greatest fear of patients after treatment for early stage cancer; what if it comes back?
NOTE: This is an important area where a simple blood test could help patients and their doctors monitor for recurrence. The big question is: will detecting a recurrence earlier lead to a longer and better life for patients?
Treatment for Metastatic Cancer: Looking for ctDNA during treatment for metastatic cancer is important for patients. Knowing their cancer is going away during treatments is meaningful. If the ctDNA is going away they can keep their treatment the same and not have to switch to a new treatment. There should be a larger portion of patients with detectable ctDNA that can be monitored.
NOTE: Looking for ctDNA during treatment for metastatic disease makes sense. Knowing a treatment is working is important, knowing when to switch to a different treatment is important.
Patients look at the benefits of a new test in a different way. Patients want a new test to be meaningful, relevant and actionable (see Box B). This may be different in different cancer types, stages and courses of treatment. There will never be one size that fits everyone in every situation. So it is important to remember to put everything in context of what it means for individual patients with cancer. Patients want to know what the new test means for them as an individual. Unfortunately, many new tests (like ctDNA tests) are not approved by looking at individuals. Tests get approved by looking at a group of patients to prove broad benefit.

One area that needs attention is the education of patients and doctors. As new ctDNA tests move forward, the education of patients and doctors about its use to improve the care of patients is important. The development of simple, clear explanations with visual graphics can help inform patients (see Box C).

It is important to manage expectations about what the test can and cannot tell patients about their cancer. Patients also need to know the chances of the test being wrong. For example, ctDNA may be present but not captured in the tube of blood being tested. Having a positive ctDNA does not mean your cancer will definitely spread. Having a negative ctDNA test does not mean your cancer will never spread. A ctDNA test could decrease as well as increase anxiety of some individual patients. So managing what the test means and doesn’t mean is important.
The potential impact of using ctDNA testing in cancer care is significant. These are some of the reasons that keep the momentum moving forward.
- It only takes a simple blood draw. Blood draws are easy, fast, inexpensive and very familiar to many cancer patients. It is also cheaper and more accessible than a body scan of any type. Finding out information about the tumor through a blood sample may eliminate the need for a biopsy. Biopsies can be costly and painful. That would be a great benefit.
- Monitoring cancer burden during treatment (response) and for recurrence can change the lives of cancer patients. It can be used throughout all the steps in the care of cancer patients.
In the end, there is a need to manage expectations about the interpretation of the ctDNA test. However, it has the potential to be meaningful, relevant, and actionable. This can help increase knowledge and reduce fears. The hope is for cancer patients to live longer and live better.
Edited by Anthony Tao

Leave a comment