Reading time: 7 minutes
Muhammad Ayhan Murtaza
A pivotal moment in the evolution of human civilization occurred when the Greek Titan Prometheus bestowed fire upon humanity, defying the will of the other gods. Today, a similar transformative force is at play with the advancement of artificial intelligence (AI). At least such is the common perception. AI is not only becoming increasingly relevant in our daily lives but is also being harnessed by pioneering researchers to enhance their work, promising to elevate the quality of human life in the times ahead. Cancer researchers are no exception.
Up until now, cancer diagnosis can revolve around PET, mammograms, MRIs, etc. However, these techniques are expensive, coarse, and yet not as precise. The precision they offer is primarily geared towards detecting cancers, often at stage 1. By that time there may already be hundreds of thousands of cancer cells, if not millions. But the elegant thing about AI is that it is precise and much more sophisticated. Let’s take a deeper dive into it.
Traditional methods, such as X-rays, CT scans, and tissue biopsies, have long been the mainstay of cancer diagnosis. These methods are reliable but not only expensive, and involve huge infrastructure and machinery. Not only that these methods are not very precise in diagnosis either. For instance, a study reported that an AI model could identify the risk of cancer in nodules with an AUC of 0.87, outperforming existing clinical tests. (Read Further: https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(22)00526-6/fulltext)
Genomic testing has also revolutionised cancer diagnosis by identifying genetic mutations in tumours. However, it often requires time-consuming and costly laboratory work, limiting its accessibility. Therefore, many of the places in the world cannot afford these costly and innately complex procedures.
Let’s take a look at a tabulated comparison of traditional methods of cancer diagnosis and potential AI-based approaches.
| Aspect | AI-Based Approaches | Traditional Methods |
| Early Detection | – AI may detect cancer at earlier stages by analyzing vast amounts of imaging data. – Identify subtle changes in scans, and thus might help us improve the sensitivity and specificity of mammograms. | – Traditional methods may miss subtle early signs. – May exhibit human error in interpretation. |
| Precision in Pathology & Personalised treatment plans | – AI may assist pathologists in accurately classifying cancer subtypes. – Reduces diagnostic errors. This might help increase efficiency in handling pathology workload.- AI might help us analyze genetic and molecular data from tumors better and faster. Thus, helping in designing personalized treatment recommendations, optimizing treatment outcomes and minimizing the side effects. IIt might also utilise patient data to assess individual risk factors and suggest early screening for high-risk individuals. | – Traditional pathology methods are generally considered reliable; however, they are susceptible to potential human errors. While these methods have been the cornerstone of diagnostic practices, the involvement of human interpretation introduces a level of uncertainty. Despite their established efficacy, the reliance on manual analysis poses challenges, and advancements in technology are continuously sought to enhance accuracy and reduce the likelihood of errors. |
| Equipment Costs | – Initial high costs for AI infrastructure and software. The necessity for ongoing maintenance and updates is a factor that should be considered. Moreover, there is potential for the reduction of labor costs through task automation. While the implementation of automated processes can lead to efficiency gains, it is essential to recognize that regular maintenance and updates may be required to ensure the sustained effectiveness of these automated systems. Balancing the benefits of reduced labor costs with the commitment to maintaining and updating automated solutions is crucial for achieving long-term operational success. – Requires skilled staff for algorithm development and maintenance. | – Lower initial equipment costs for traditional methods. – Ongoing maintenance may be necessary, but less technology-dependent. – Involves higher labor costs due to the need for skilled healthcare professionals to perform diagnostic tasks. |
| Patient Outcomes and Treatment Costs | – Improved early detection can lead to cost savings by reducing late-stage treatments.- Can reduces the cost of misdiagnosis and thus, may reduce administrative costs | – Late-stage treatments are often costlier and have a lower chance of success. |
| Sensitivity | – Potentially high sensitivity, capable of detecting subtle changes in medical images. – Might assist in identification of early-stage lesions or abnormalities that may be missed by the human eye. | – Sensitivity may vary based on the type of traditional method used (e.g., X-rays, CT scans, or biopsies). – Some methods may have lower sensitivity for early detection. |
| Speed of Analysis | – Potential rapid analysis of vast datasets, leading to quicker results. – Suitable for handling large volumes of data efficiently.- Can process a large number of cases, making mass screenings more feasible. | – Traditional methods may require more time for image analysis or laboratory tests, potentially delaying the diagnosis. |
| Tumor Characterization | – AI can potentially assist in characterizing tumors at an early stage, helping to identify their nature and behavior. | – Traditional methods may primarily focus on tumor detection and may provide limited information on tumor characterization. |
Interesting Examples:
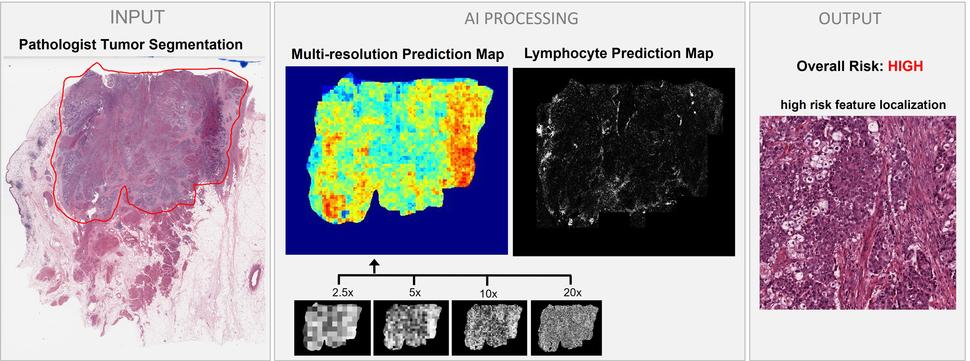
Some examples that really showcase the true potentials of AI in diagnostic oncology include a chip that was developed by the lab of the oncology giant, Professor Dr Bert Vogelstein. The small chip can detect the earliest markers (or signs) of more than 16 different types of cancer in a few drops of blood! Another lab came up with an AI model that uses digital images of bladder tumour tissue sample (“INPUT” on the left) to predict the risk of the cancer spreading to nearby lymph nodes (“OUTPUT” on the right).
Credit: Courtesy of Stephanie Harmon, Ph.D via. NIH newsletter. (https://www.cancer.gov/news-events/cancer-currents-blog/2022/artificial-intelligence-cancer-imaging)
Hurdles to Overcome
Although the potential of AI is immense, there are yet some hurdles that need to be overcome in order to unleash the potential of AI in its entirety.
1. Data Challenges: AI’s performance depends on access to diverse and large datasets, which may not be readily available for all cancer types or demographics. Gathering such data requires collaboration among healthcare institutions and may raise privacy concerns. Many parts of the world are seriously underrepresented across the domains of medicine and especially oncology where the sophisticated deciphering of genotypes and/or pathogenic causes needs rather intricate and expensive machinery.
2. Privacy and Ethical Concerns: Patient data privacy and security must be a top priority and therefore poses an immense ethical dilemma. Developing robust safeguards and adhering to stringent regulations is essential to address these concerns.For example, Target infamously disclosed a daughter’s pregnancy to her father before he was aware, and Amazon’s Alexa mistakenly furnished a user’s transcripts and audio files to an unintended recipient. (Read further; https://www.forbes.com/sites/kashmirhill/2012/02/16/how-target-figured-out-a-teen-girl-was-pregnant-before-her-father-did/?sh=51b757786668) These incidents unequivocally constitute privacy breaches, both attributable to AI. Target and Amazon’s Alexa transgressed customers’ privacy by divulging information to unauthorized parties without their explicit consent. Despite AI’s intent to leverage this data for value creation, it inadvertently encroached upon individuals’ fundamental right to privacy.
3. Validation and Clinical Integration: AI algorithms need rigorous testing and validation to ensure their reliability and safety. Clinical integration, including training healthcare professionals to use AI tools effectively, is necessary. A total integration of AI into hospitals would initially cost a lot, let alone training doctors and healthcare professionals to get the best out of these technologies. This, again poses a not-so-different problem to the third world as compared to the ones they are faced with right now.
4. AI-Human Collaboration: AI should complement, not replace, human expertise. Collaboration between AI and medical professionals is crucial to ensure the best possible care for patients. AI with all its potential, in its current form represents a non-evolving system which is not of much consequence if not complemented with the wisdom of human judgement.
Conclusion
The role of AI in oncology diagnosis presents exciting prospects for the future of cancer care, as it offers the potential for earlier detection, precise pathological analysis, and personalized treatment recommendations. However, the journey ahead is marked by significant hurdles, including data limitations, privacy concerns, and the need for validation and integration into clinical workflows that are yet to be overcome.
To harness the full potential of AI in oncology, stakeholders must work together to overcome these hurdles, ensuring that AI complements human expertise while upholding patient rights and maintaining the highest standards of care. With a thoughtful and collaborative approach, AI can be a valuable ally in the ongoing battle against cancer, providing hope and improved outcomes for patients worldwide.
Edited by Shan Grewal
References
- Brito-Rocha T, Constâncio V, Henrique R, Jerónimo C. Shifting the Cancer Screening Paradigm: The Rising Potential of Blood-Based Multi-Cancer Early Detection Tests. Cells. 2023 Mar 18;12(6):935. doi: 10.3390/cells12060935. PMID: 36980276; PMCID: PMC10047029.
- Hunter B, Hindocha S, Lee RW. The Role of Artificial Intelligence in Early Cancer Diagnosis. Cancers (Basel). 2022 Mar 16;14(6):1524. doi: 10.3390/cancers14061524. PMID: 35326674; PMCID: PMC8946688.
- Jaber, Nadia. “Can Artificial Intelligence Help See Cancer in New, and Better, Ways?” https://www.cancer.gov/news-events/cancer-currents-blog/2022/artificial-intelligence-cancer-imaging
- Iliashenko O, Bikkulova Z, Dubgorn A. Opportunities and challenges of artificial intelligence in healthcare. InE3S Web of Conferences 2019 (Vol. 110, p. 02028). EDP Sciences.
- Racine E, Boehlen W, Sample M. Healthcare uses of artificial intelligence: Challenges and opportunities for growth. InHealthcare management forum 2019 Sep (Vol. 32, No. 5, pp. 272-275). Sage CA: Los Angeles, CA: SAGE Publications.
- https://www.theguardian.com/society/2023/apr/30/artificial-intelligence-tool-identify-cancer-ai

Leave a comment