Reading time: 4 minutes
Indiwari Gopallawa
After years of seminal research work, mRNA technology got its moment as a result of the Covid-19 pandemic. However, mRNA-based cancer vaccines remain a relatively new and untapped class of vaccines that show great potential. The enthusiasm for this novel technology has been increasing due to recently published experimental studies that show the effectiveness of mRNA vaccines against several types of cancers.
What is the role of Messenger RNA (mRNA) in a cell?
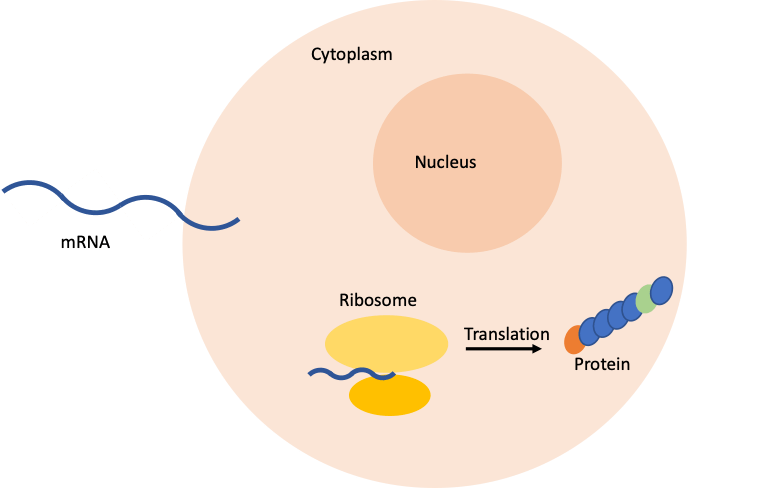
mRNA is transcribed from a DNA template and plays a role in protein synthesis. The function of mRNA is to pass information from the DNA inside the nucleus of a cell to the cytoplasm of a cell, where protein synthesis occurs. An organelle known as a ribosome, reads the mRNA sequence and translates each of three nucleotides known as a codon into its matching amino acid and makes a peptide chain that eventually becomes a protein.
Why mRNA-based vaccines are beneficial against cancer?
The purpose of mRNA-based vaccination is to activate the immune system to eliminate cancer cells in a different way than other therapies as discussed earlier on OncoBites. Vaccines can be produced to target cancer-associated antigens, specifically proteins that are specifically present in cancer cells but not in normal cells. Once vaccinated, the body will produce antibodies that will help eliminate cancer cells. Interestingly, vaccination can help maintain memory cells in the immune system to achieve sustained cancerous cell killing. In addition to activating the immune system, mRNA vaccines have several advantages such as mRNA molecules are considered non-infectious and the production of mRNA vaccines is relatively inexpensive and fast.
How do mRNA vaccines work?
A strand of synthetic mRNA goes into the cell and the corresponding protein is made by the ribosomes (Figure 1). These proteins get taken up by dendritic cells (cells that can display part of the foreign protein to immune cells to educate them) that break down the proteins into smaller fragments known as peptides. These peptide-antigens then get displayed to immune cells such as T cells. T cells can signal B cells to differentiate into plasma cells that produce antibodies that are specific to the foreign protein. In other words, the peptide fragments generated from the synthetic mRNA are recognized by the immune system as foreign and T cells kill the infected cells. Further, immune cells that are activated by an antigen can provide memory so that in case the foreign substance comes back, the immune system is ready to attack!
Efficacy of mRNA vaccines in clinical trials
Recently, there is a steady increase in the number of clinical trials with mRNA-based cancer vaccines. Results from a Phase I study published in the journal of clinical investigations demonstrated an increase in the number of tumor-specific T-cells (T cells are a part of the adaptive immune system and can initiate an immune response against cancer/tumor) by injecting a single mRNA molecule to vaccinate patients with gastrointestinal cancer. Another similar study in Phase II demonstrated that administering melanoma patients with an mRNA-based vaccine against antigens expressed on melanoma cancer cells increased specific T-cell responses showing the effectiveness of mRNA vaccines.
Future of mRNA vaccines
The recent development of mRNA vaccines against SARS-CoV-2 has significantly highlighted the huge potential of mRNA-based treatment options. The U.S. Food and Drug Administration (FDA) has approved two vaccines to treat cancers against human papilloma virus (HPV) and hepatitis B virus (HBV). An mRNA cancer vaccine developed by Moderna and Merck recently has shown positive results in melanoma patients in Phase II clinical trial study. At the time of writing this article, the FDA has not approved any mRNA-based cancer vaccine despite the considerable progress of mRNA-based vaccines in clinical trials, and the success of COVID-19 vaccines. One of the main challenges in generating mRNA-based cancer vaccines is identifying individual cancer-related antigens or neoantigens (proteins on cancer cells). Additionally, it has been shown that the vaccine injection site is a critical component that determines mRNA distribution and efficacy. Although, clinical trials of mRNA-based cancer vaccines are encouraging, according to a recent article published by authors at the University of Pennsylvania, further improvements in the mRNA delivery methods and a complete understanding of the mechanisms of action are needed to increase the efficacy of mRNA-based vaccines while minimizing adverse events. Despite these challenges, the potential for mRNA-based cancer vaccines is promising.
Edited by Ifeoluwa Oyelade
References Discussed:
- Lorentzen CL, Haanen JB, Met Ö, Svane IM. Clinical advances and ongoing trials on mRNA vaccines for cancer treatment. Lancet Oncol. 2022;23(10):e450-e8. Epub 2022/09/30. doi: 10.1016/s1470-2045(22)00372-2. PubMed PMID: 36174631; PMCID: PMC9512276.
- Cafri G, Gartner JJ, Zaks T, Hopson K, Levin N, Paria BC, Parkhurst MR, Yossef R, Lowery FJ, Jafferji MS, Prickett TD, Goff SL, McGowan CT, Seitter S, Shindorf ML, Parikh A, Chatani PD, Robbins PF, Rosenberg SA. mRNA vaccine-induced neoantigen-specific T cell immunity in patients with gastrointestinal cancer. J Clin Invest. 2020;130(11):5976-88. Epub 2020/10/06. doi: 10.1172/jci134915. PubMed PMID: 33016924; PMCID: PMC7598064.
- Miao L, Zhang Y, Huang L. mRNA vaccine for cancer immunotherapy. Molecular Cancer. 2021;20(1):41. doi: 10.1186/s12943-021-01335-5.

Leave a comment