Reading Time: 3 minutes
Libby-Ann Harpaul-Sahadeo
Chemotherapy is a drug treatment that uses powerful chemicals to kill fast-growing cells in the body. It is most often used to treat cancer. Taxanes are a class of chemotherapy drugs used to treat many types of cancer, including ovarian, breast, lung, cervical, endometrial, gastroesophageal, and head and neck cancers.
Taxanes work by inhibiting the function of cytoskeletal microtubules in cancer cells. By binding to microtubules, taxanes interfere with the formation of the mitotic spindle. The mitotic spindle is a structure made of fibers that help separate chromosomes during cell division to ensure each new cell gets the right number of chromosomes. Stopping the mitotic spindle from forming and preventing the breakdown or separation of microtubules prevents the cancer cell from being able to divide (mitosis). This eventually leads to cell death (apoptosis).
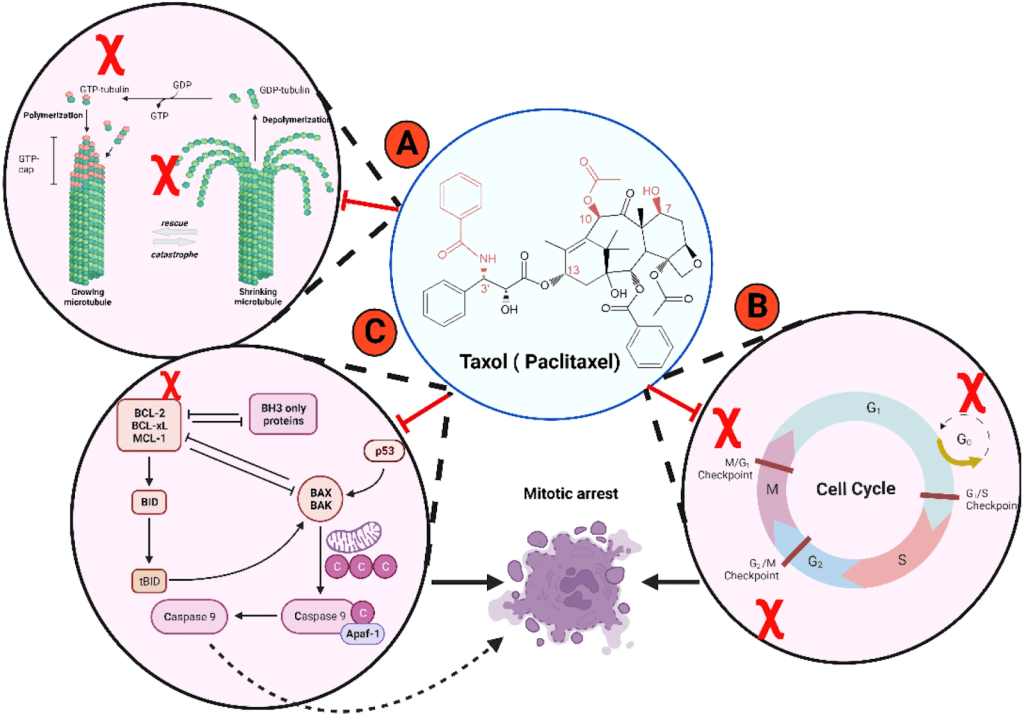
Figure 1. Example of Taxane drug mechanism of action.
Taxane is given in intravenous (IV) formulation in a dosage format, and the correct dosage is crucial to ensure the drug works effectively. Dosage calculation can be done accurately by understanding drug elimination. Understanding drug elimination, primarily measured by clearance (CL) and half-life is crucial for accurate dosage calculation because it determines the maintenance dose needed to achieve a safe and effective steady-state concentration and dictates the appropriate dosing interval
It’s also based upon the demographics of patients, such as the type of cancer that patients have, their age, and pre-existing conditions.
However, traditional body surface area can (BSA) based dosing of cytotoxic drugs fails to capture the intricate ways these drugs are processed by the body, resulting in inconsistent drug levels and effects. While overdosing is readily apparent, underdosing, which may go unnoticed, could affect 30% or more of patients on standard treatment. This inadvertent underdosing can significantly compromise the drug’s cancer-fighting ability.
Still, overdosing is a major problem, and the way that taxane toxicity manifests depends on the specific taxane administered. “Effects of paclitaxel toxicity include cardiac conduction abnormalities, specifically bradycardia, alopecia, nail discoloration, and rarely hepatitis and pneumonitis. Docetaxel leads to characteristic fluid retention, skin toxicities, and stomatitis. Effects of cabazitaxel toxicity include infections, nausea, vomiting, diarrhea, and constipation. A lack of hypersensitivity reactions characterizes nab-paclitaxel but can cause nausea and vomiting, alopecia, arthralgia, myalgia, and elevation of liver enzymes.
Though taxane toxicity may be extreme, it can be reversed with appropriate management. Typical docetaxel regimens include 3-weekly infusions, and prophylactic steroids are recommended for 72 hours, starting 24 hours before the drug administration. Paclitaxel-induced bradycardia is usually an incidental finding and doesn’t typically require cardiac monitoring during treatment. Often, no active intervention or consultation with a cardiologist is necessary. For taxane-related arthralgia and myalgia, flupirtine may be a good treatment option.
While the management of taxane toxicity is currently a necessary, yet reactionary, measure, the future of this crucial chemotherapy class hinges on precision: researchers are rapidly developing and integrating strategies like Model-Informed Precision Dosing (MIPD) and pharmacogenomics (PGx) to calculate individualized doses a priori, ensuring patients receive the optimal therapeutic exposure needed to maximize cancer treatment efficacy and preemptively minimize severe side effects.
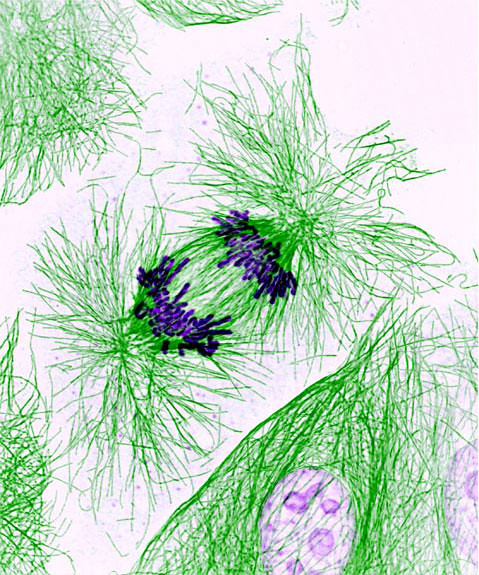
Header Image Source: https://www.flickr.com/photos/nihgov/20062504363/
Figure 1 Source: https://cancerci.biomedcentral.com/articles/10.1186/s12935-024-03415-0/figures/2
Edited by Jessica Desamero
References
Taxol (Paclitaxel) mechanism of action in cancer. (2024). Cancer Cell International, 24(1), Article 280. https://cancerci.biomedcentral.com/articles/10.1186/s12935-024-03415-0/figures/2
Drugs.com. (n.d.). Paclitaxel Dosage. Retrieved October 20, 2025, from https://www.drugs.com/dosage/paclitaxel.html
Horde, G. W., & Gupta, V. (2024). Drug Clearance. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557758/#:~:text=Clearance%20is%20equal%20to%20the,clearance%20from%20all%20other%20tissues.
Horde, G. W., & Soni, P. (2023). Taxane Toxicity. StatPearls Publishing. Retrieved from https://pubmed.ncbi.nlm.nih.gov/36943973/#:~:text=Cabazitaxel%20toxicities%20include%20infections%2C%20nausea,and%20elevation%20of%20liver%20enzymes.
Miyakis, S., & Pefani, D. (2017). Pharmacogenetic and Pharmacokinetic Dose Individualization of the Taxane Chemotherapeutic Drugs Paclitaxel and Docetaxel. Current Clinical Pharmacology, 12(3), 162–171.https://www.benthamscience.com/article/84364#:~:text=Price%3A%20%2465-,Abstract,suboptimal%20dosing%20for%20many%20patients.
Oosting, S. F., de Vries, J., Lub-de Hooge, M. N., de Jonge, M. E., Beukers, M. W., & de Koning, E. B. (2025). From Prospective Evaluation to Practice: Model-Informed Dose Optimization in Oncology. Clinical Pharmacokinetics. https://pmc.ncbi.nlm.nih.gov/articles/PMC11946950/#:~:text=MIPD%20in%20oncology.-,Model%2DInformed%20Precision%20Dosing,2%20and%203).
The Taxanes. (2000). In E. Frei III & J. F. Holland (Eds.), Holland-Frei Cancer Medicine (5th ed.). B. C. Decker. https://www.ncbi.nlm.nih.gov/books/NBK13728/#:~:text=Interest%20in%20the%20taxanes%20began,activity%20in%20preclinical%20tumor%20models.&text=In%201971%2C%20Wall%20and%20coworkers,constituent%20of%20the%20bark%20extract.
Pharmacogenomics | Genomics and Your Health.” Centers for Disease Control and Prevention. https://www.cdc.gov/genomics-and-health/pharmacogenomics/index.html
Pérez-Blanco, Jonás Samuel, and José M Lanao. “Model-Informed Precision Dosing (MIPD). Pharmaceutics, vol. 14, no. 12, 6 Dec. 2022, editorial. https://pmc.ncbi.nlm.nih.gov/articles/PMC9780803/.

Leave a comment