Reading time: 5 minutes
Joycelyn Ghansah, MA, MPH
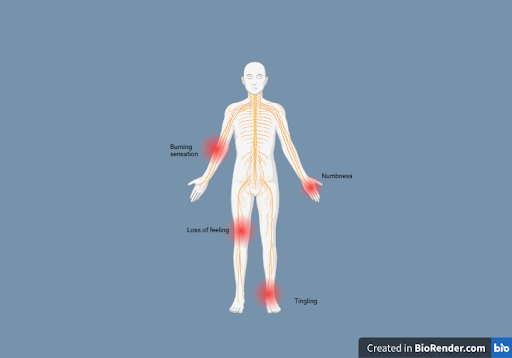
Chemotherapy-induced peripheral neuropathy (CIPN), or neuropathic pain (pain due to nerve damage), is a common type of pain experienced by cancer patients, especially those receiving treatment. It happens due to the side effects of cancer drugs, which affect 19% to over 85% of patients. CIPN mostly causes sensory issues, sometimes in the brain and neck, and can also lead to problems with movement and other bodily functions, with varying levels of intensity and duration.
Neuropathic pain can affect a patient’s overall quality of life by influencing their daily interactions with family and friends, work, eating habits, and mental and emotional well-being. An analysis revealed that about 59% of patients receiving cancer treatment reported pain, along with 64% of patients with advanced disease and 33% of patients after treatment. Effective palliative care is important for improving quality of life and survival. It focuses on managing pain by addressing patients’ physical, mental, and emotional needs. Neuropathic pain in cancer patients can be complex to treat because it is often caused directly by the cancer damaging the nerves, such as when cancer places pressure on the nerve or nervous system. Additionally, the potential side effects of chemotherapy or surgery may damage the nerve. Therefore, finding effective treatment methods is crucial. Undermanagement can cause serious harm and worsen other cancer-related issues. Effective pain management is crucial for cancer patients dealing with neuropathic pain, as it enhances their quality of life and overall well-being.
Gabapentin and CIPN
The importance of relieving pain and the availability of effective therapies underscore the need for healthcare providers to be skilled in cancer pain assessment and treatment. Providers may recommend various options, including radiotherapy-induced nerve damage interventions and opioid medications such as tramadol and tizanidine. However, Gabapentin is a well-known anticonvulsant drug with analgesic effects, has been proven effective for reducing cancer pain, and is considered a better alternative to opioids for cancer patients receiving radiation.
The effects of Gabapentin are well-known in conditions such as post-herpetic neuralgia, painful diabetic neuropathy, spinal cord injury pain, and neuropathic cancer pain. More common cancer-related neuropathic pain syndromes are listed in Table 1. The use of Gabapentin in patients with neuropathic pain can alleviate pain and increase daily activity.
| Table 1: Neuropathic pain syndromes ——————————————————————————————— Plexopathies Cervical plexopathy Malignant brachial plexopathy Malignant lumbosacral plexopathy Sacral plexopathy Coccygeal plexopathy Painful peripheral mononeuropathies Paraneoplastic sensory neuropathy Leptomeningeal metastases Painful cranial neuralgias Glossopharyngeal neuralgia Trigeminal neuralgia Malignant painful radiculopathy |
Gabapentin in clinical trials
Trials conducted in 2013 indicated that the use of Gabapentin for neuropathic cancer pain is well established, with the number needed to treat (NNT) ranging from 4.2 to 6.4. Patients and survivors often report rapid relief within the first or second week of treatment. The goal of pain management is not only to reduce adverse events and increase pain relief but also to avoid addiction-related outcomes and enhance daily activities and movement. Recent studies have shown that Gabapentin effectively manages neuropathic cancer-related pain more frequently than opioids such as fentanyl and tramadol. Although there is limited evidence regarding the ineffectiveness of Gabapentin once treatment has stopped, many studies demonstrate a significant reduction in cancer-related neuropathic pain during Gabapentin treatment. Some possible side effects of Gabapentin, as shown in Table 2, may resolve on their own or improve with a change in dosage.
| Table 2: Side effects of gabapentin for patients with neuropathic pain Somnolence and dizziness are the most common side effects Peripheral edema Weight gain Nausea Vertigo Asthenia Dry mouth Ataxia |
Additional benefits include improved sleep and increased daily activity in patients with severe neuropathic pain. Even with low doses of 100mg to 300mg, patients saw improvement in their pain. Although Gabapentin does not increase food intake, its use can help alleviate the severe pain that often results in reduced appetite, making it difficult to eat or swallow. This is especially true for cancer patients suffering from neuropathic pain in the head and neck.
Gabapentin is one of the most effective treatments for managing patients with neuropathic cancer pain, particularly those who have already been treated with opioids, as well as patients and survivors who have experienced undertreatment. Studies have shown that the long-term effects of using Gabapentin can reduce the need for high doses of opioids, as its analgesic effects target neuropathic nerve damage resulting from cancer treatment. This ultimately improves the quality of life for patients and survivors, especially those with head and neck cancer.
Additionally, studies indicate that a combination of opioids and Gabapentin can help to alleviate severe cancer pain, allowing for better pain management. It is important to note that it can have side effects; some long-term effects remain unknown. Therefore, healthcare professionals must monitor its effects and assess patient use of Gabapentin.
Header Image Source: Created by author in Biorender.com
Edited by Jessica Desamero
References
- Chen, Dong-Liang MDa; Li, Yu-Hong MD, PhDa,b,*; Wang, Zhi-Juan MDc; Zhu, Ye-Ke MDa,b. The research on long-term clinical effects and patients’ satisfaction with gabapentin combined with oxycontin in the treatment of severe cancer pain. Medicine 95(42):p e5144, October 2016. | DOI: 10.1097/MD.0000000000005144
- Mulvey, M. R., Paley, C. A., Schuberth, A., King, N., Page, A., & Neoh, K. (2024). Neuropathic Pain in Cancer: What Are the Current Guidelines? Current Treatment Options in Oncology, 25(9), 1193. https://doi.org/10.1007/s11864-024-01248-7
- Swarm, R. A., Paice, J. A., Anghelescu, D. L., Are, M., Bruce, J. Y., Buga, S., Chwistek, M., Cleeland, C., Craig, D., Gafford, E., Greenlee, H., Hansen, E., Kamal, A. H., Kamdar, M. M., LeGrand, S., Mackey, S., McDowell, M. R., Moryl, N., Nabell, L. M., Nesbit, S., BCPS, O’Connor, N., Rabow, M. W., Rickerson, E., Shatsky, R., Sindt, J., Urba, S. G., Youngwerth, J. M., Hammond, L. J., & Gurski, L. A. (2019). Adult Cancer Pain, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw, 17(8), 977-1007. Retrieved Mar 5, 2025, from https://doi.org/10.6004/jnccn.2019.0038
- Zajączkowska, R., Kocot-Kępska, M., Leppert, W., Wrzosek, A., Mika, J., & Wordliczek, J. (2019). Mechanisms of Chemotherapy-Induced Peripheral Neuropathy. International Journal of Molecular Sciences, 20(6), 1451. https://doi.org/10.3390/ijms20061451

Leave a comment