Time to read: 5 minutes
Chris Wang
Long before the T-cell was discovered, an American surgeon and cancer researcher named William Coley laid the groundwork for harnessing the immune system to attack cancer. His successful treatment of a patient with inoperable sarcoma by injecting heat-inactivated bacteria into the tumor later became known as “Coley’s Toxins”. Despite not knowing the exact mechanism behind its efficacy, Dr. Coley correlated treatment benefit with the ability of his toxins to induce a fever. Although Coley’s toxins ultimately fell out of favor compared to chemotherapy and radiation, Dr. Coley’s research was later credited as a precursor to modern-day immunotherapy.
These modern-day immunotherapy agents include intravesicular BCG vaccine, interferons, interleukins, and PD-1/PD-L1 immune checkpoint inhibitors. While each agent is important, many researchers consider PD-1/PD-L1 inhibitors to be the most impactful due to its ability to improve the overall survival of many different solid tumor types. As of September 2024, there are over a dozen immune checkpoint inhibitors approved by the Food & Drug Administration (FDA) for dozens of solid tumors including those listed in Figure 2. Although sarcomas were one of the first tumor types to demonstrate success with Coley’s toxins, immune checkpoint inhibitors have largely failed in trials that enrolled sarcoma patients. With the exception of the extremely rare subtype, alveolar soft part sarcoma (which represents only <1% of all cases), treatment for most sarcomas do not include immune checkpoint inhibitors. Hypotheses for these disappointing results include low tumor immunogenicity, anti-inflammatory cytokines, immunosuppressive macrophages, and a lack of objective biomarkers to select sarcoma subtypes that may benefit.
Figure 2. Word Cloud of FDA Approved Indications for PD-1/PD-L1 Inhibitors in Solid Tumors
Sarcomas are a very rare group of heterogeneous cancers (over 70 subtypes) that account for only 1% of adult cancers but 15% of childhood malignancies. They can be divided into sarcomas of the soft tissues (which includes fat, muscle, and nerves), as well as bone sarcomas. While the standard of care for localized disease remains surgery with or without radiation and possibly chemotherapy, advanced stage sarcomas have an extremely poor prognosis and are generally treated with chemotherapy alone. Response rates for anthracycline-, ifosfamide-, or gemcitabine-based regimens in the first-line setting for metastatic soft tissue sarcomas are less than 30% with a median overall survival of less than 2 years. To improve upon these poor outcomes, novel treatments with durable responses are desperately needed.
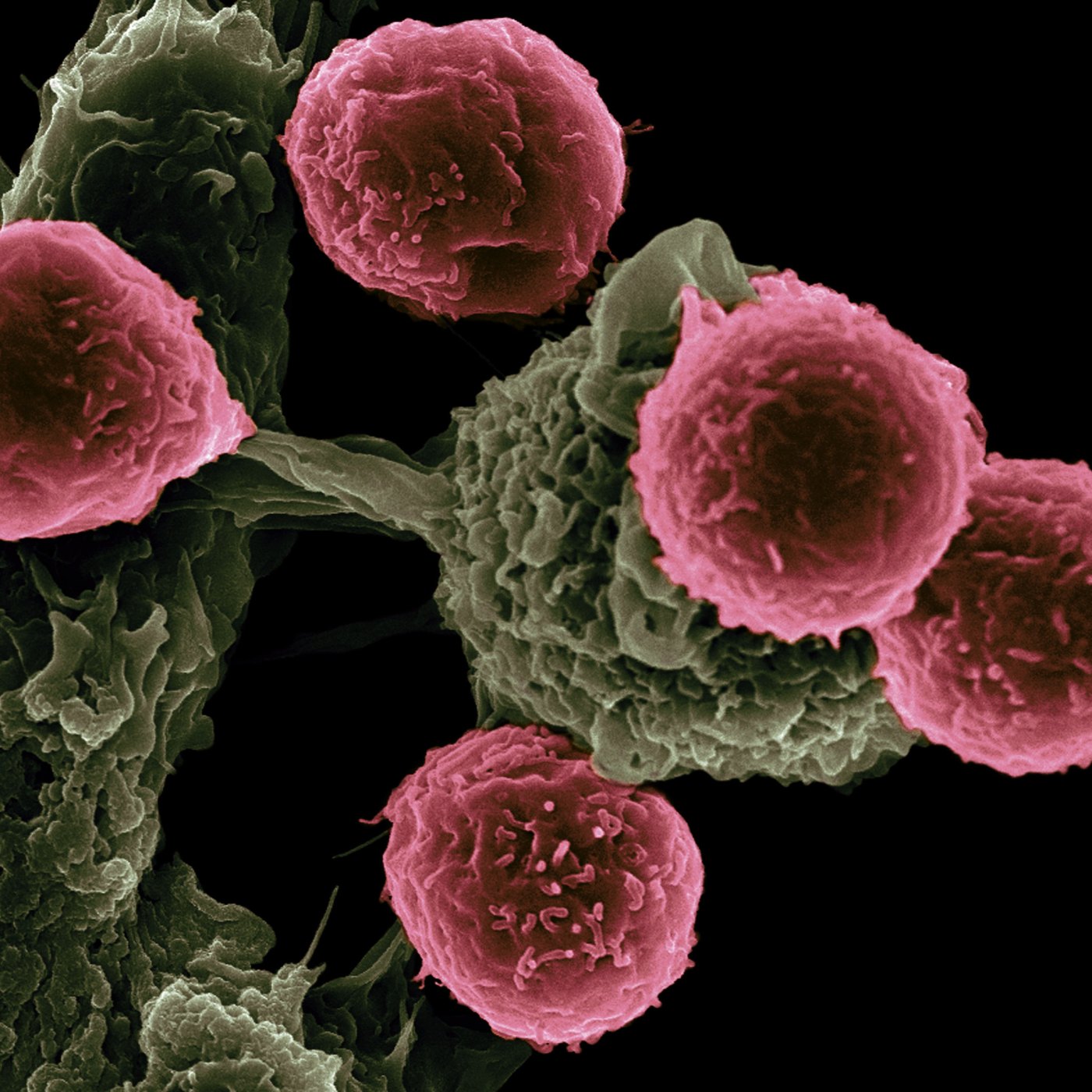
Adoptive cellular therapies have transformed the treatment of relapsed/refractory leukemias, lymphomas, and myeloma. This type of immunotherapy involves taking a patient’s own T-lymphocytes, modifying them to recognize a cancer antigen, and then reinfusing the cells back into the patient. In August 2024, the FDA granted approval for afamitresgene autoleucel (afami-cel), an adoptive cell therapy for advanced synovial sarcoma, based on the results of the phase 2 SPEARHEAD-1 trial. In this trial, 52 patients with advanced stage synovial sarcoma had their T-cells collected, transduced with a lentiviral vector to express an affinity enhanced T-cell receptor against the tumor antigen MAGE-A4, expanded ex-vivo, and then reinfused after lymphodepletion. Synovial sarcomas represent 5-10% of all soft tissue sarcomas and almost universally express the intra-cellular MAGE-A4 protein that are presented on MHC-class I protein complexes (Figure 3). Despite enrolling heavily pre-treated patients, the trial found a response rate of 39% and a median overall survival of over 15 months. Given the <20% response rates seen with the historical standard of care in the relapsed refractory setting for synovial sarcoma, the results of this trial support the use of afami-cel as a second line of therapy.
Figure 3. Representation of Engineered Adoptive T-Cell Therapy Targeting MAGE-A4
Immunotherapies have revolutionized the treatment of many solid tumor types but for far too long most sarcoma subtypes have not been included. With the newest approval of afami-cel, decades of failure have given way to success and renewed excitement for immunotherapy in sarcoma is growing. Ongoing research is looking to expand afami-cell to other sarcoma subtypes as well as study other cellular therapies targeting separate sarcoma antigens such as NY-ESO-1. The field has grown tremendously since William Coley and his tube of dead bacteria, and with hard work and dedication, new and innovative solutions will continue to be discovered to fully harness the power of our immune system to combat cancer.
Abbreviations: PD1/PDL1: programmed cell death protein 1, programmed death ligand 1, d-mmr: mismatch repair deficient, msi-h: microsatellite instability high, SCLC: small cell lung cancer, SCC: squamous cell carcinoma, NSCLC: non-small cell lung cancer, MAGE4: melanoma-associated antigen 4, MHC: major histocompatibility complex, NY-ESO-1: New York esophageal squamous cell carcinoma 1
Header image credit: Victor Segura Ibarra and Rita Serda, Ph.D., National Cancer Institute, National Institutes of Health
Edited by Nicholas Egan
References
- Coley WB. The Treatment of Inoperable Sarcoma by Bacterial Toxins (the Mixed Toxins of the Streptococcus erysipelas and the Bacillus prodigiosus). Proc R Soc Med. 1910;3(Surg Sect):1-48.
- Fazel M, et al. Immunotherapy for Soft Tissue Sarcomas: Anti-PD1/PDL1 and Beyond. Cancers (Basel). 2023;15(6):1643.
- Seddon B, et al. Gemcitabine and docetaxel versus doxorubicin as first-line treatment in previously untreated advanced unresectable or metastatic soft-tissue sarcomas (GeDDiS): a randomised controlled phase 3 trial. Lancet Oncol. 2017 Oct;18(10):1397-1410.
Judson I, et al.. Doxorubicin alone versus intensified doxorubicin plus ifosfamide for first-line treatment of advanced or metastatic soft-tissue sarcoma: a randomised controlled phase 3 trial. Lancet Oncol. 2014 Apr;15(4):415-23. - D’Angelo SP, et al. Afamitresgene autoleucel for advanced synovial sarcoma and myxoid round cell liposarcoma (SPEARHEAD-1): an international, open-label, phase 2 trial. Lancet. 2024 Apr 13;403(10435):1460-1471.

Leave a comment